In 1962, Howard and Norma Lotsof stumbled on the fact that ibogaine can help with opioid addiction.
Then, for 60 years, researchers have studied ibogaine’s effects on addiction to opioids and cocaine. They’ve consistently found that ibogaine can help with the cravings, withdrawals, sadness and depression that come along with opioid and cocaine addiction.
But ibogaine researchers haven’t studied alcohol very much. That’s despite the fact that alcohol is the drug of abuse that’s most commonly used by most people. And the fact that alcohol can actually do as much damage as opioids or cocaine.
Today, Beond is helping fill the gap in scientific knowledge about ibogaine and alcohol.
We conducted our own research study. Our simple question was: can ibogaine contribute to recovery from alcoholism? Our findings are striking.
Guests with alcohol dependency who went through our treatment program said they left feeling happier, less anxious, and with fewer withdrawal symptoms.
Note: Our study shows preliminary patient outcomes, which need to be further validated through the peer-review process. But we wanted to share our initial findings with our community.
Here are the basics of our research study, in plain English.
What Alcohol Dependency Is
Alcohol Dependency occurs when people feel like they need to drink, even when they know it can harm their health, relationships, or daily responsibilities. They may ignore liver damage or lost income. They might even hide flasks from loved ones, sneak sips between business meetings, or chug liquor in the bathroom.
Seventeen percent of Americans binge drink, and seven percent drink heavily. Drinking too much kills three football stadiums worth of people each year.
For many, stopping drinking can feel as difficult as stopping breathing, or giving up sunshine. Why? There are social, physical, and emotional challenges. First, if everyone around you is drinking, it’s hard to be the odd one out. Second, if you quit, there are withdrawal symptoms—especially if you’re a super-heavy drinker. Third, if you do quit, anxiety and depression are common, making recovery even harder.
Worse, traditional treatments, such as medication, twelve-step programs, and behavioral therapy, for alcohol dependency are often under-utilized due to stigma or a shortage of professional support. Relapse rates are around 60 percent.
All these negative effects leave room for relapse.
What Ibogaine Is
Our study explores the efficacy of ibogaine in treating alcohol dependency.
Ibogaine is a psychedelic substance from the African plant Tabernanthe iboga.
It’s traditionally used in Central Africa by the Fang, Pygmy, and Babongo tribes for spiritual ceremonies in their Bwiti religion. For them, iboga is akin to communion wine.
Ibogaine came to light in the West in the 1960s, after a couple named the Lotsofs found ibogaine eased the cravings for opioids. One dose of ibogaine, they found, and a person might no longer be dopesick.
There have been a few promising signs that ibogaine could treat alcoholism. Studies in rodents show that ibogaine can reduce self-administration of alcohol. And small case studies of humans, including veterans, suggest ibogaine can help reduce troublesome alcohol use.
Medical Care is Key
Our ibogaine treatments last about 12 hours. They can be risky, as ibogaine can cause severe side effects like an irregular heartbeat, especially in people with pre-existing heart conditions. Ibogaine can also cause nausea, vomiting, and dizziness. That’s why it’s important for a study of ibogaine to happen at a place like Beond.

We are a well-equipped medical facility with some of the best ibogaine doctors and nurses. We carefully screen our guests to make sure they’re fit for treatment. And we monitor the whole person—especially their hearts—during and after their ibogaine sessions to make sure our guests stay safe.
Study Goals
For this study, we closely observed the impact of ibogaine treatment on patients with alcohol dependency as they stopped using the drug. We wanted to see if ibogaine could lessen their withdrawal symptoms and improve their mental health.
Who Was in Our Study
Fifty-eight guests (21 women and 37 men) who had alcohol dependency took part. The average age of patients was 39 years. Our guests had to have signs of misuse, including difficulty in cutting back or feeling the need for treatment.
To be considered as having alcohol dependency, patients needed to be drinking heavily. That means at least four drinks three times per week for the last six months. On average, patients reported they drank about 6 days a week, having 7 drinks per day. That’s 42 drinks a week. On average, they had been struggling with alcohol misuse for nearly 20 years.
Before starting treatment, guests were asked to avoid alcohol for a week. Not all managed to do so.
How We Measured Guests’ Troubles
Upon their arrival and prior to departing Beond, each guest completed the following surveys twice to assess their anxiety, depression, and withdrawal symptoms before and after ibogaine treatment.
— The Beck Anxiety Inventory: A survey with 21 questions asking questions about anxiety like: “How often do you feel heart pounding, hands trembling, or fear of dying?”
— The Beck Depression Inventory: Another 21-question survey asking about depression. People reported their depressive thoughts, such as “I am so sad and unhappy I can’t stand it,” “I feel I am a complete failure as a person,” and “I would kill myself if I had the chance.”
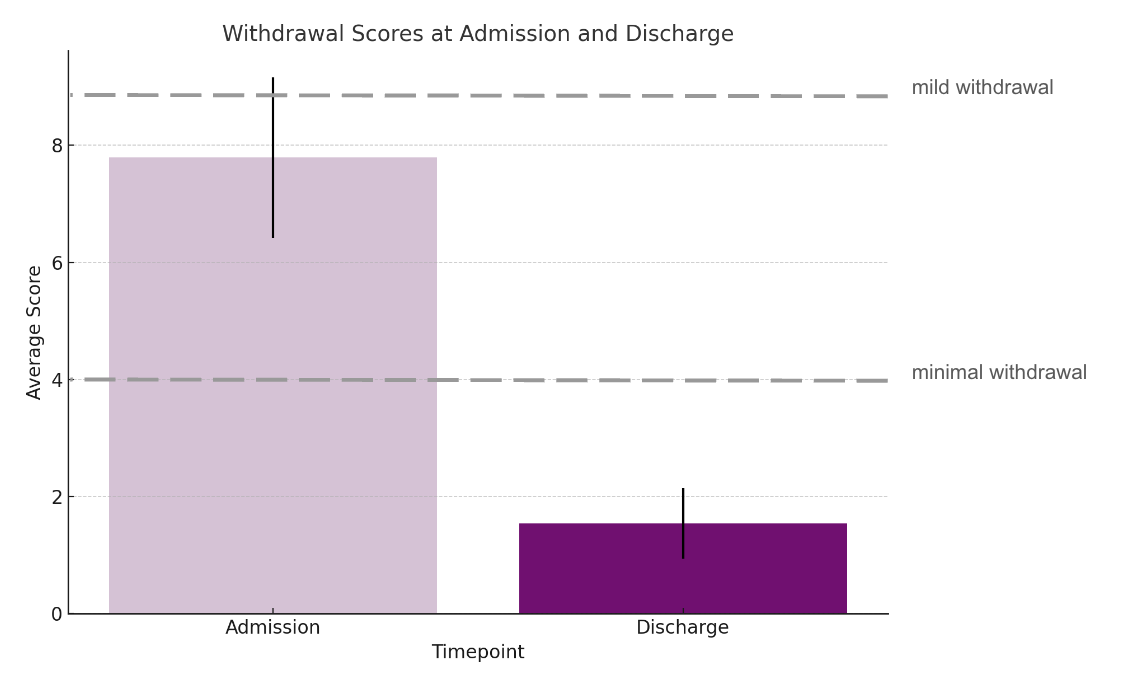
— Clinical Institute Withdrawal Assessment of Alcohol Scale, Revised: People who are quitting alcohol report whether they feel nausea, itching, pins and needles, whether their arms are trembling, or whether they even know what day it is—all typical signs of alcohol withdrawal.
Treatment Process
The study participants went through the typical Beond program. Each did a 10 or 14-day inpatient program at our clinic in Cancun, Mexico, sometime between March 2022 and March 2024.
They received comprehensive medical and psychological care. Each guest had heart monitoring, blood tests, and drug screenings. Patients who could abstain from alcohol for a week before arriving had a slightly shorter treatment duration—10 days instead of 14.
On treatment days, patients received doses of ibogaine. The amount was carefully calculated based on factors like age, weight, and medical history. The average dose was 8–12 mg per kg of body weight. Patients were monitored closely for 12 hours, as ibogaine can affect the heart. After treatment, patients participated in counseling, well-being activities, and discharge planning. For some, additional smaller doses of ibogaine, called “boosters,” were administered.
Study Finds Less Anxiety, Depression and Withdrawal
After the treatments, we studied the survey responses. How did our alcohol-dependent guests feel before going through our ibogaine treatments? And how did they feel afterward? Was there a difference?
The results were promising. Across the three key areas—anxiety, depression, and withdrawal—patients experienced notable improvements.
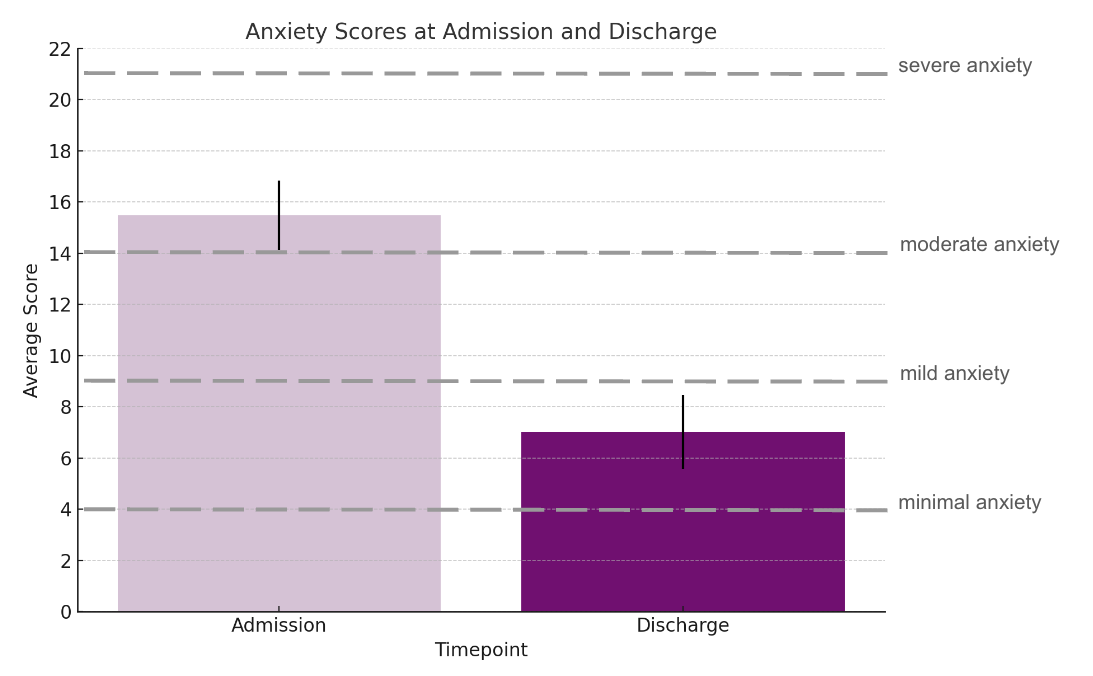
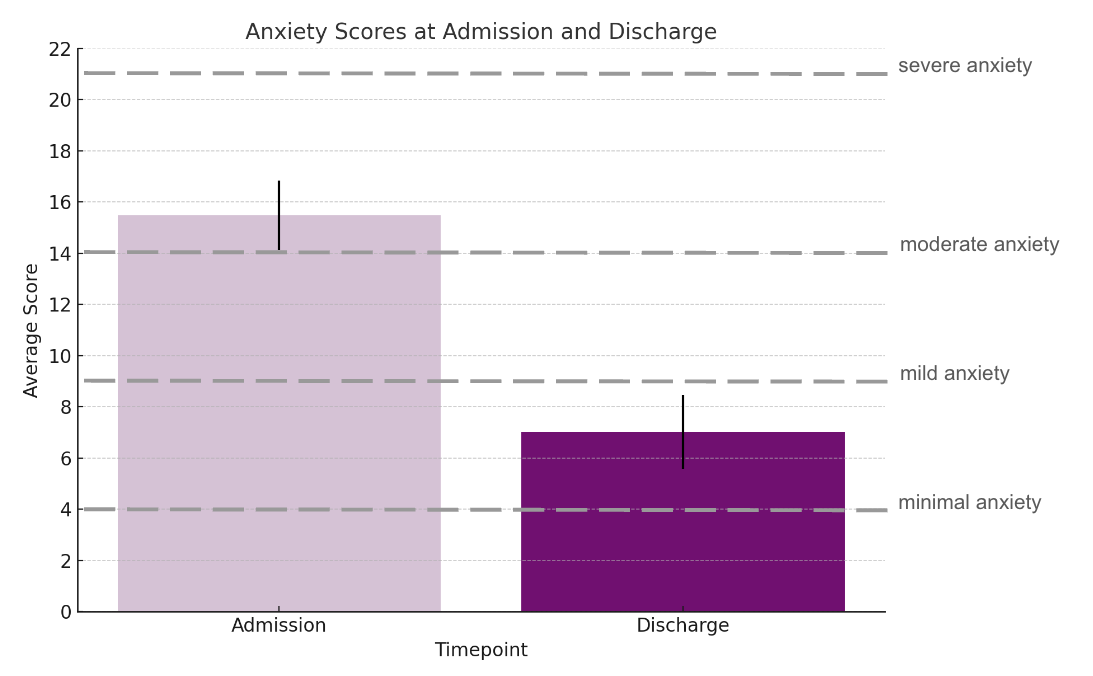
Anxiety
At the start, according to the survey, guests’ anxiety levels were moderate. By the end, most had minimal or no anxiety symptoms. Overall, their anxiety scores on the surveys dropped by nearly half, showing a 49% average improvement.
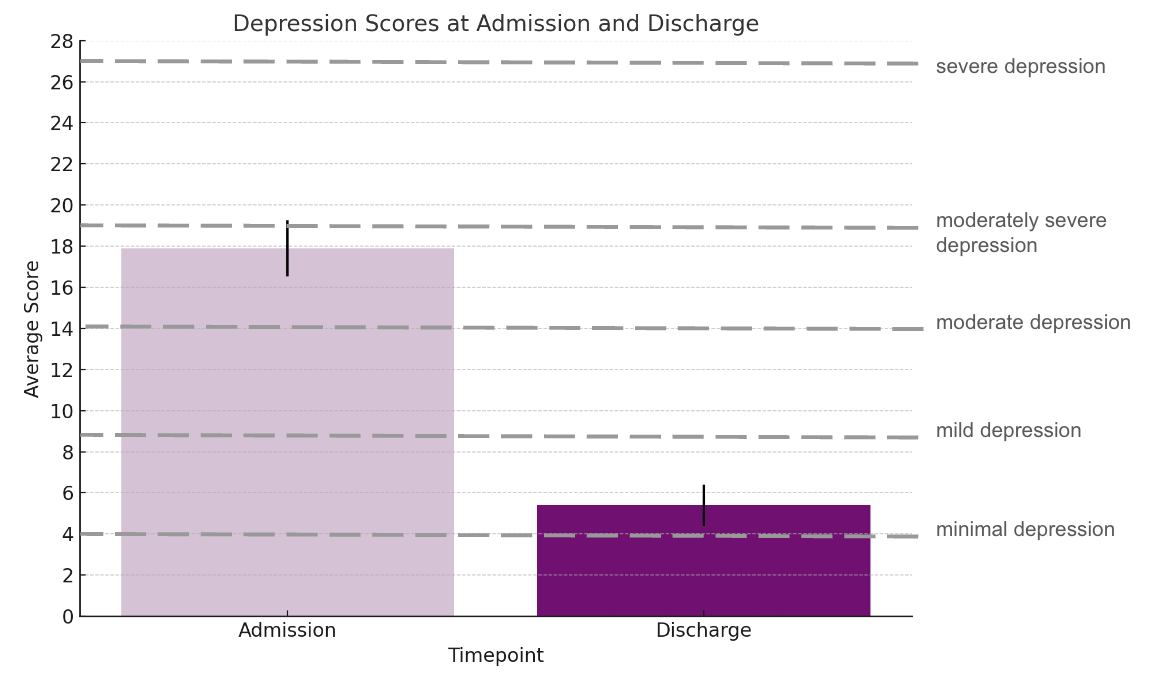
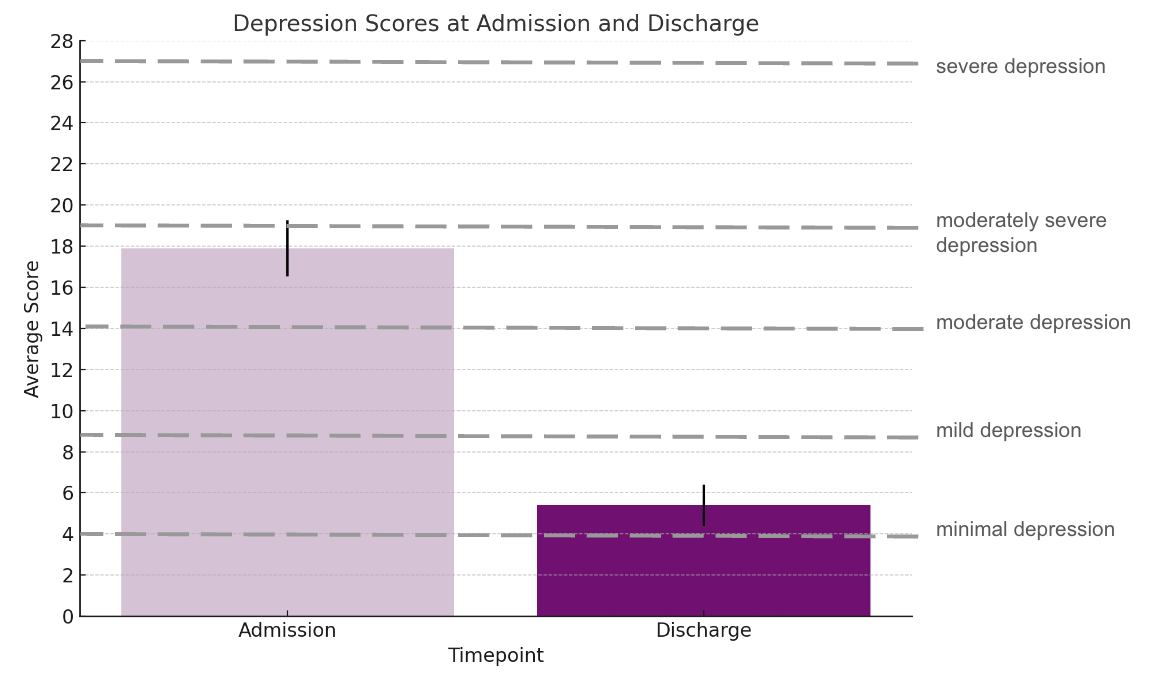
Depression
Depression scores also significantly decreased by 69%. Guests, on average, went from having “moderate to moderately severe” depression to having “minimal to mild” depression or not being depressed at all.
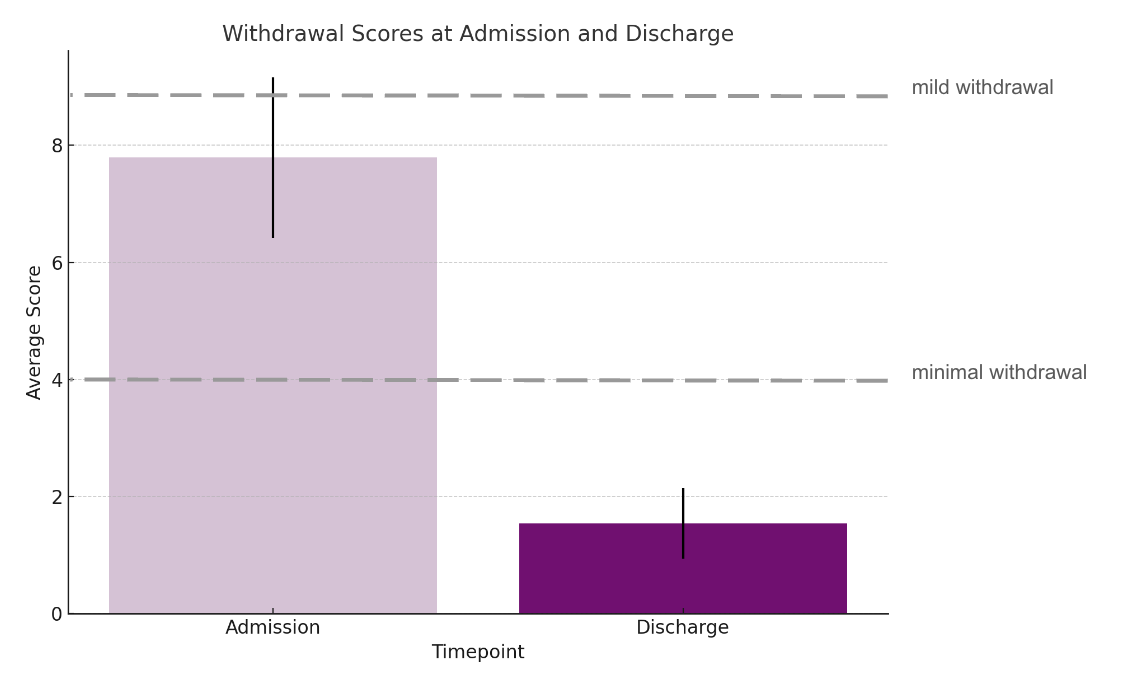
Withdrawal
For many patients, alcohol withdrawal symptoms went from “mild” at the start to “minimal” or “none” by the end, with an average 77% reduction in alcohol withdrawal symptoms.
Simply put, our guests went home feeling less anxious and depressed than when they arrived. And they had far fewer alcohol withdrawal symptoms.
The Big Takeaway
The findings support our hunch that ibogaine could effectively reduce both the mental health symptoms and withdrawal symptoms of alcohol dependency. Being calmer and happier could improve patients’ commitment to treatment and reduce the likelihood of relapse. The study suggests ibogaine could be an effective part of a larger approach to recovery from alcoholism.
Why Ibogaine May Work
Ibogaine appears to create a “neuroplastic” effect in the brain. Ibogaine opens a “critical period” where the brain is more adaptable to forming new habits and changing old ones. This could help patients reshape their relationship with alcohol, making it easier to resist cravings or relapses.
Compared to other psychedelics like psilocybin (which opens these critical periods for about two weeks), ibogaine’s effects seem to last for up to four weeks, and clients continue receiving benefits from ibogaine treatment for up to three months, offering a longer time period for recovery and healing.
This study also aligns with research on psychedelics like MDMA and psilocybin. When combined with therapy, these drugs have been shown to help people with substance use disorders. Each psychedelic works a bit differently, but all seem to help address trauma, regulate emotions, and reduce addiction-related stress.
Ibogaine specifically appears to help people reflect on their lives and choices.
With this deeper understanding, people can understand the root causes of their addiction, and make changes.
Limitations of the Study
Every research study will have some limitations, which are important to disclose. Self-reported data, like surveys, can introduce biases. Guests may alter their answers—unintentionally or intentionally—to suit the story they’d like to tell themselves, or the story they think their doctors, nurses and researchers would like to hear. As well, guests who voluntarily and willingly seek ibogaine treatment for alcohol dependency to get better may differ from those who do not seek such treatment.
Conclusion
Ibogaine seems to have potential as a treatment for alcohol dependency by helping manage cravings, withdrawal, anxiety, and depression. Our findings suggest ibogaine could be a valuable option for people seeking new approaches to recovery from alcohol misuse.