A bomb goes off. Life drastically changes. Recovery feels like an infinite mile away.
Growing up in the Southern United States, John* was surrounded by a large group of childhood friends and supportive parents. Following in his father’s military footsteps, he enlisted in the armed services, going on three deployments over eight years.
While on patrol, his vehicle hit an improvised explosive device (IED). The blast claimed the lives of all other people on board except for his.

Surviving the Aftermath: TBI, PTSD, and Opioid Dependency
The severity of his injuries required doctors to place him in an induced coma to reduce brain swelling, while surgeons worked to remove shrapnel and repair multiple injuries.
Diagnosed with traumatic brain injury (TBI) and PTSD, John’s life changed. Night after night, he managed only two to three hours of sleep, plagued by vivid nightmares. Severe headaches resulting from his TBI with no effective treatment solutions sidelined him from social and family life.
Prescribed Percocet for pain management, John eventually developed a dependency and found himself taking twice his prescribed dose.
Simple everyday sounds such as babies crying and crowded areas would trigger intense anxiety. His friends and his wife witnessed his uncontrolled explosiveness, especially after a few drinks, and grew anxious, too. His friendships frayed and his options dwindled.
Discovering Ibogaine
Then, a beacon of hope emerged: a fellow veteran told him about ibogaine treatment. Ibogaine is a psychedelic drug derived from a plant native to Central West Africa.
What sets ibogaine apart from other psychedelics is that it is non-addictive and non-recreational.
The trip lasts for about 12 hours, and it is not often a nice one because it elicits profound introspection that some may find “brutally honest” and “uncomfortable1,2.” With his employer’s sponsorship, John traveled to Beond in Cancún, Mexico, in the summer of 2024.

A Transformational Experience at Beond
John’s time at Beond was intense and emotional, which was something he hadn’t expected. During the treatment, he described witnessing toxins being purged from his body. In his vision, he rediscovered his lost soul, he said, which appeared to him as his teenage self.
Just three days after treatment, John’s sleep quality transformed from two to three hours to a full eight to ten hours per night. His pain completely disappeared. His neurologist noted that two regions of his brain affected by TBI appeared to have decreased in size in monthly fMRI scans—suggesting actual brain repair taking place.
Tom Feegel, CEO of Beond, describes John’s transformation as, “He went from down in the dumps to rising like a phoenix.”
Dr. Shirley Cheung, Beond’s director of research, was drawn to John’s story. She documents John’s remarkable journey to healing in a groundbreaking new case study to be published. Her case study and John’s story offers hope to thousands of others who carry similar invisible wounds of war. And it couldn’t come at a better time. TBI has emerged as the signature injury of post-9/11 military conflicts, affecting tens of thousands of service members and veterans.
The Bigger Picture: The Cost of TBI on Veterans
The impact on military personnel is both widespread and costly. Veterans with TBI face medical expenses nearly four times higher than those without, averaging $5,831 annually compared to $1,547 in 2009. Traditional treatments, while beneficial for specific symptoms, have shown limited success in providing comprehensive, long-term relief. Most troublingly, many veterans report feeling abandoned by the very medical system meant to support them.
Ibogaine’s Role in Healing the Brain
A small but growing number of TBI survivors are turning to ibogaine. On a scientific level, ibogaine may help TBI by increasing important brain growth factors called GDNF and BDNF. These stimulate the growth of new brain cells and neural connections. Additionally, ibogaine interacts with NMDA receptors in the brain, which are involved in pain signaling. By modulating these receptors, ibogaine can help reduce chronic pain and decrease hyperexcitability in pain pathways.
John saw dramatic improvements in his case, and the transformative effects of ibogaine can vary from person to person. For John, the most striking changes were in his family life. The man who said he had never been emotional before treatment found himself able to connect deeply with others. He now reports that he can show up as a present father. His wife remarked that he had transformed into a different and better version of himself.
Fifteen weeks after treatment, John, 44, remains pain-free and opioid-free, with no cravings. He maintains his well-being through practices learned at Beond, including stretching, meditation, and breathwork. His short-term memory has improved so significantly that he no longer needs to write things down to remember them. Most importantly, he’s regained his ability to engage with the world around him, free from the debilitating anxiety that once controlled his life.
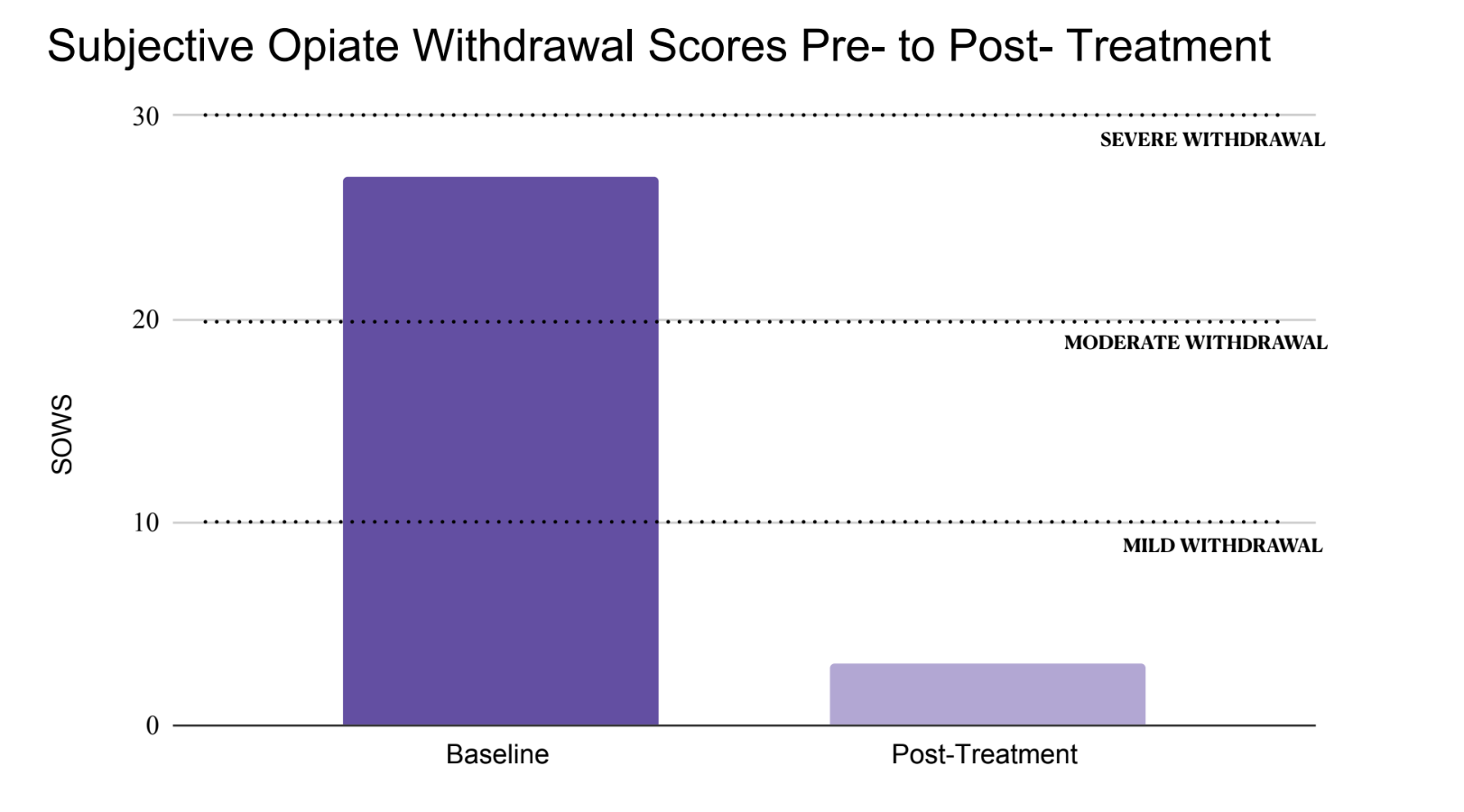
John experienced moderate to severe opioid withdrawal symptoms before ibogaine treatment. After treatment, his symptom score dropped by 89%, reaching minimal withdrawal by the final day of the 10-day Opioid Treatment program.
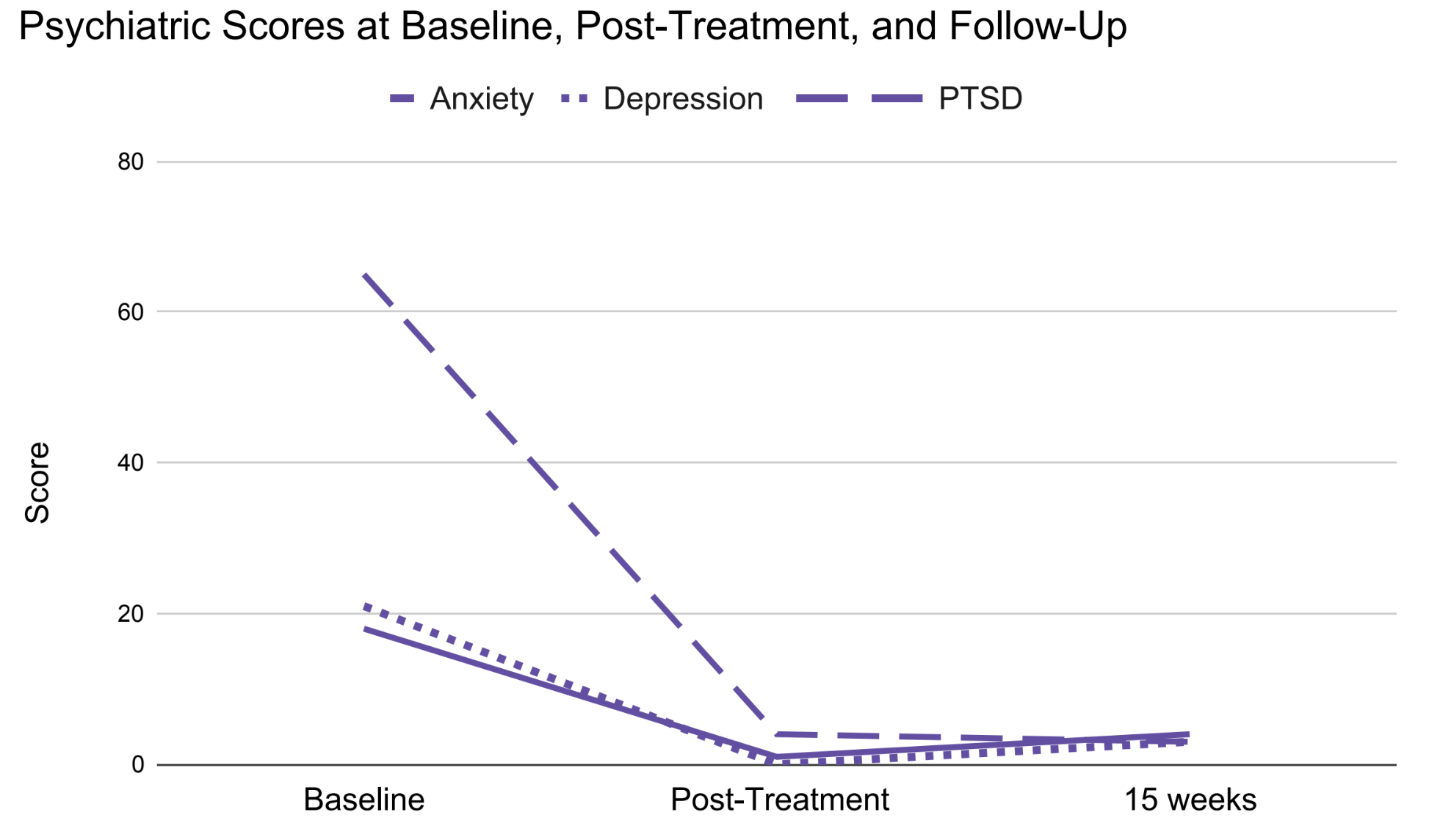
John’s scores for Anxiety, Depression, and PTSD showed substantial improvement following ibogaine treatment, remaining stable at 15 weeks after completing the program, with reductions of 78%, 86%, and 95%, respectively.
The Future of Ibogaine Research and Accessibility
“John’s case was unbelievable,” Dr. Cheung said. “Here was a person who had almost lost all hope, who had depleted all their resources trying to get better. It is remarkable to see his ailments relieved—the pain gone, the anxiety improved, the drug cravings eliminated, and the quality of sleep restored.”
While ibogaine shows promise in treating conditions like TBI, PTSD, and addiction, it remains classified as a Schedule I substance in the United States, meaning it cannot be legally prescribed or administered.
One of Beond’s initiatives is to produce high-quality research and collaborate with policymakers and the community to correct any misconceptions about ibogaine and work towards increasing accessibility for those desperately in need of a solution for their pain.
A Call for Change
To Dr. Cheung, John’s journey represents a beacon of hope for veterans struggling with the complex aftermath of combat trauma. While his story is unique, it highlights the potential of innovative treatments in addressing the often overwhelming challenges faced by those carrying the unseen wounds of war. And, it may hint at the need for changes in the law in the United States. As Dr. Cheung notes, “It’s finally time that these veterans who have sacrificed so much for people to live good lives in America be taken care of by Americans.”
* Name changed to protect privacy.
1. Alper KR, Beal D, Kaplan CD. Chapter 14 A contemporary history of ibogaine in the United States and Europe. In: The Alkaloids: Chemistry and Biology. Vol 56. Academic Press; 2001:249-281.
2. Brown TK. Ibogaine in the treatment of substance dependence. Curr Drug Abuse Rev. 2013;6(1):3-16.
3. Taylor BC, Hagel EM, Carlson KF, et al. Prevalence and Costs of Co-occurring Traumatic Brain Injury With and Without Psychiatric Disturbance and Pain Among Afghanistan and Iraq War Veteran VA Users. Medical Care. 2012;50(4):342-346.